A Science-based Approach to Curb Your Alcohol Cravings
We prescribe medications that are scientifically proven to suppress cravings and improve your relationship with alcohol–and deliver them straight to your door.
Baclofen
Baclofen is an FDA-approved medication traditionally used to treat muscle spasms, and is prescribed off-label due to one interesting side-effect: it helps users suppress alcohol cravings, and break their drinking habit.
How we use baclofen
Based on the Ameisen Method, we begin by prescribing a low dose of baclofen to new participants.
Users may drink normally as we follow-up to check for reductions in alcohol cravings and drinking.
Finally, we gradually increase the dose until an effective dose is discovered that makes users completely and effortlessly indifferent to alcohol.
How does baclofen work?
Baclofen is the go-to treatment for AUD in France, Australia, and here at LifeBac. It’s been prescribed for decades and is known to be totally safe.
“No medication works effectively for everyone, and baclofen is surely no exception... So far it seems to work in all types except for one, and that’s people who turn up once and don’t come again. But it’s not one size fits all; you have to refine it. Not to say that I’m a great doc, but every time I’m on the case I’ve yet to find a patient where it’s not a success. I’ve been playing with this medication for 10 years.”
Baclofen, like any medication, induces a variety of different responses in every new person that takes it. Some people report life-changing differences even at small doses, while others see no discernible changes; some people have intolerable (yet temporary) side effects, while most have none; some people don’t even notice that they’re drinking less and find themselves shocked at how much they’ve naturally reduced over time. Everyone’s reaction to baclofen is unique to their own biology and lifestyle.
Although baclofen has been used extensively for decades for muscle spasticity, so we have a lot of data on its potential side effects, it is now off-patent and its use for alcohol treatment is off-label, so there’s little financial incentive for pharmaceutical companies to fund studies into its effectiveness. This means that, until recently, there were very few legitimate, large-scale studies into baclofen’s efficacy as an addiction treatment. Luckily, alongside baclofen’s surge in popularity in Europe, Australia, and numerous other countries, there has been a marked increase in the amount of research being done.
The first randomized, placebo-controlled study of baclofen titrated using the Ameisen Method was the BACLAD study, published in 2015. Even though this study treated anything but total abstinence as a failure, the baclofen group still achieved a remarkable 68% success rate, almost three-times the 23% rate of the placebo group. In 2018, another French study, OBADE-ANGH, reported 70% success in reducing to safe drinking levels and 44% success in maintaining complete abstinence among its 214 participants.
The BACLAD study, presented in 2016 at the Berlin World Congress on Alcohol and Alcoholism, analyzed 320 high-risk drinkers (averaging 13 standard drinks per day), and is praised for its inclusiveness and realistic methods, spanning 60 general practices with no exclusions for pre-existing medical conditions. Excluding drop-outs who didn’t complete the study, 81% of participants in the baclofen group (non-placebo) had succeeded in reducing to at least low-risk drinking levels (2/day for women, 4/day for men).
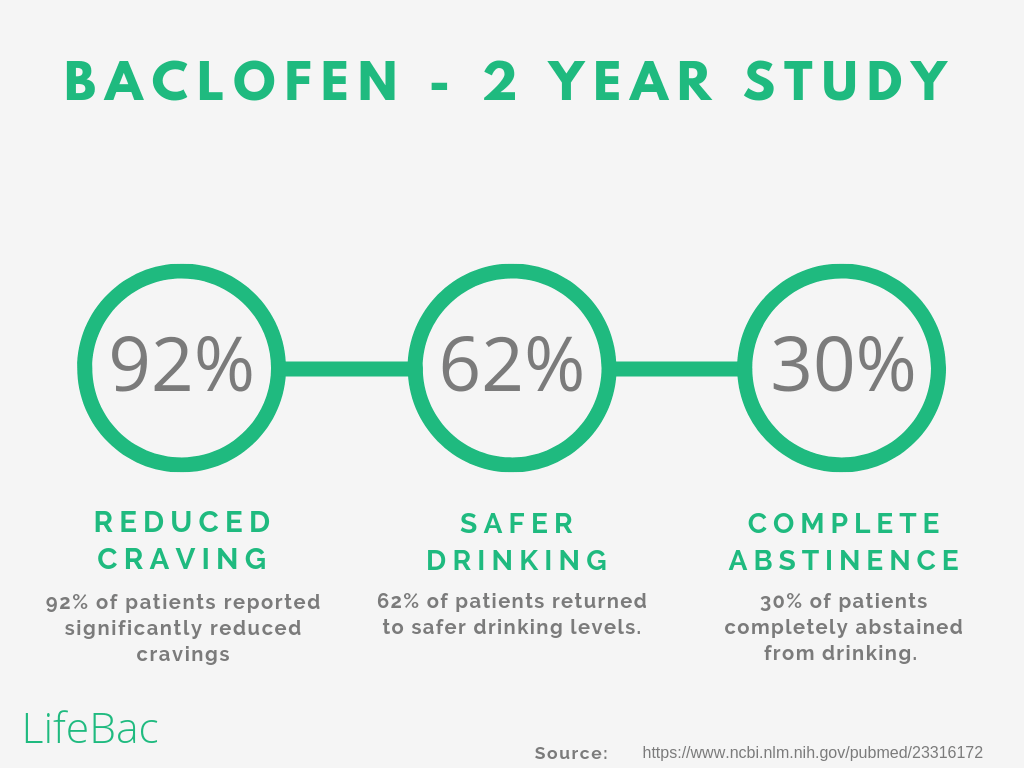
In 2012, Dr. Renaud de Beaurepaire analyzed 100 alcohol-dependent high-risk drinkers for two years as they were treated with baclofen in a non-randomized, non-placebo-controlled trial. 84% of participants showed a reduction in drinking (from high-risk to at least moderate-risk) 3 months in, and 62% maintained that reduction all the way to the 2-year mark. By the end of the two year study, half of the participants had reduced from high- to low-risk drinking or abstinence, with 70% of the remaining half of participants having discontinued treatment.
On the other hand, however, there are studies that found baclofen’s effectiveness to be minimal. Almost all of these studies had one or more obvious flaws that led to this conclusion, but they’re worth discussing nonetheless. Two other, smaller studies presented alongside the Bacloville study at the Berlin World Congress on Alcohol and Alcoholism concluded that baclofen showed little difference with the placebo. Both studies required 20 weeks total abstinence as the criterion for success, counting any reduction short of long-term abstinence as a failure. One of these, the Alpadir study, funded by European pharmaceutical giant Ethypharm, had a 40% drop-out rate and ambiguous methodology and sample; it found no difference between baclofen and the placebo. The other study, led by Dutch researchers, somehow achieved an incredible 65% success rate for achieving continuous abstinence in the placebo group who received no meaningful treatment, matching the 65% success rate of the baclofen group and leading the researchers to conclude no difference against the placebo.
The results of baclofen treatment studies over the past few years have been remarkable, but skepticism is natural: can a simple pill really cure a problem that has plagued mankind for millenia? It’s important to recognize what baclofen is and isn’t capable of; baclofen suppresses cravings, urges, and subliminal trigger responses for alcohol in the human brain. While cravings are usually the primary symptom of AUD, baclofen has no control over the original cause: your environment. The root cause of excessive drinking almost always lies in environmental factors: maybe you learned as a teenager that alcohol can make you more confident and sociable, or you formed a habit of drinking every night to unwind from a stressful work environment. The key to highly effective baclofen treatment is to take advantage of baclofen’s suppression of subconscious urges to work on unwinding your habit loops, dealing with environmental stressors, and getting better acquainted with your brain’s habit and reward circuits.
Common Reasons for Treatment Failure
While the results discussed above are certainly remarkable, there are still a minority of baclofen users who either fail to significantly reduce their drinking, or choose to prematurely stop treatment. Let’s go over some of the most common reasons baclofen doesn’t work.
The most common reason for stopping baclofen treatment prematurely is side effect management. Baclofen’s most common side effects are nausea, dizziness, tiredness, and insomnia, although more severe effects like paresthesia (tingling), tinnitus, hallucinations, and mania have been reported in very rare cases. For the vast majority of people, side effects are very mild and only occur on dose increases; slowing down titration will usually mitigate side effects. Unfortunately, because baclofen treatment in the U.S. is often done independently, and people with AUD are very likely to also suffer from anxiety, people are much more likely to be scared off of baclofen after experiencing mild side effects at low doses, and they’re much less likely to understand that adjusting their titration can end their experience of unwanted side effects. Here at LifeBac, we pay close attention to the appearance of side effects, especially in the early stages of treatment, and can almost always solve the issue of unwanted side effects with slight titration schedule adjustments.
Another surprisingly widespread cause of failed baclofen treatment is people just not taking their baclofen. With Alcohol Use Disorder especially, it’s quite common for people to be “forced” into treatment by an ultimatum from their partner or family, usually with the traditional expectation of total lifelong abstinence as the goal. In these cases, the user is not internally motivated to continue treatment, and might actually have the opposite motivation; this is just another reason that self-empowerment, goal-setting, and personal control over treatment are core principles of the LifeBac program. People who aren’t genuinely motivated to improve themselves might purposely fail their treatment — whether consciously or subconsciously — so that they can rationalize returning to excessive drinking. People who are forced into treatment are also likely to be. It’s also quite common for people who aren’t used to taking regular medication, take a wide range of medications, or are frequently intoxicated, to simply forget to take their baclofen or accidentally dose themselves incorrectly. Other people may have a psychological issue with having to take medication at all. At LifeBac, we make your comprehensive titration plan readily available to you through the app and web portal, as well as encouraging you to track your medication doses taken in the app’s Agenda View and regularly checking in with semi-weekly Progress Reports.
The other major cause of baclofen treatment failure is when AUD is heavily enforced by environmental factors — even more so than internal urges or cravings. If alcohol is an important part of your culture, family, or social and professional lives, it can seem impossible to cut down even with baclofen suppressing your cravings. Baclofen can only affect you; it has no power over your family, home life, or external pressures to drink. This is what LifeBac’s success guiding program is all about; our LifeBac Guides are trained to help you use the increased autonomy and mental clarity that baclofen’s suppression of cravings provides in order to properly deal with the external stressors that led to your excessive drinking in the first place.
For the most part, the cause of failed baclofen treatment is either unrealistically high expectations of the medication — baclofen takes time, it won’t cure you overnight, and it can’t change your environment aside from making you more capable of doing so yourself — or a lack of motivation on behalf of the user.
Baclofen was introduced for sale in 1974 as an antispasmodic medication to reduce muscle spasticity caused by issues in the brain or spinal cord. Its lack of severe side effects made it an excellent alternative to the most popular antispasmodic at the time, Valium. Baclofen quickly caught on and has now seen widespread use for the past 45 years in patients with spinal cord injuries, ALS, and multiple sclerosis.
Baclofen’s use in reducing alcohol consumption was discovered around the year 2000, when the French Dr. Olivier Ameisen, who was himself a severe treatment-resistant alcoholic who had been given five years to live, prescribed himself baclofen and eventually described himself as “completely and effortlessly indifferent to [alcohol].” Baclofen now has hundreds of thousands of users in France and is the first-line treatment for over-drinking, but is still gaining traction in the United States. Baclofen reduces or even eliminates the cravings and withdrawal symptoms associated with reducing your drinking. It has no impact on your body’s response to alcohol, like Antabuse, and is most effective when taken regularly throughout the day.
The human brain contains GABA receptors which, when bound with a neurotransmitter called GABA, regulate feelings of fear or anxiety, among other things. Alcohol is so similar to the GABA neurotransmitter that it can actually take its place and bind with GABA receptors in the brain when we drink — that’s why alcohol can give us more confidence by reducing anxiety and fear. When drinking heavily and consistently, however, alcohol works so well as a GABA agonist that the brain slowly stops producing actual GABA, allowing alcohol to take its place. When problem-drinkers then try to cut back or quit, the brain isn’t capable of making the proper amount of GABA, which can cause anxiety and depressive symptoms as well as intense cravings for alcohol.
Baclofen is a derivative of GABA; just like alcohol, it binds to GABA receptors in the brain, but without the serious health implications of consistent alcohol use. By stimulating the brain’s GABA receptors, baclofen stops the brain from craving alcohol to accomplish the same job. European studies have concluded that once they’ve reached their effective dose, which generally takes between 1 and 3 months, 92% of “high-risk” drinkers report an effortless reduction in drinking. Even though it essentially replaces alcohol’s role as a GABA agonist, baclofen does not seem to be addictive, and doesn’t cause cravings, but shouldn’t be quit cold-turkey for risk of side effects.
Baclofen’s interaction with GABA is also the source of its anxiolytic (anti-anxiety) properties. Anxiety disorders are very strongly associated with excessive drinking, and the co-occurrence of anxiety and Alcohol Use Disorder is remarkably common. Not only are people with anxiety disorders much more likely to over-drink as a method of self-medication, but anxiety is one of the most prevalent symptoms of regular excessive drinking; the two conditions maintain and amplify one another in a “vicious cycle of comorbidity.” Baclofen’s effectiveness as an anxiolytic medication further suppresses cravings for alcohol and provides some of the same anxiety relief as alcohol does without all of the negative side effects.
Alongside reducing cravings and anxiety, baclofen has also been shown to significantly slow down the brain’s subconscious reaction to visual triggers. Dr. Anna Rose Childress of the University of Pennsylvania’s Perelman School of Medicine used MRI’s to analyze the brain activity of cocaine-dependent men in response to key visual stimuli — images of drug use, paraphernalia, and preparation, as well as other aversive images. These were shown for only 33 milliseconds before switching to non-related pictures, far too quickly for the brain to consciously process the image. Fascinatingly, even these incredibly quick flashes are subconsciously interpreted by the brain as addiction triggers, and caused a significant reaction in the reward and motivational centers of the brain.
Taking just 60mg of baclofen caused a remarkable reduction in the reward and motivational brain response to ultra-fast subliminal addiction cues in cocaine-dependent addicts. While this study focused on cocaine addiction rather than AUD, and the sample size was quite small and homogenous (20 cocaine-dependent men aged 18-55), the results are remarkable, and demonstrate a whole new factor of baclofen treatment for addiction. For split-second visual triggers, baclofen suppresses the brain’s craving response; for longer cues, baclofen gives the brain time to consciously process the trigger and make a legitimate decision, rather than instantly setting off subconscious urges for alcohol.
Because baclofen is processed and absorbed by the body very quickly, it usually needs to be taken three times throughout the day to remain effective. Fortunately, this absorption takes place in the kidneys, not the liver like most other drugs, rendering baclofen the only major AUD treatment drug that can still be taken by people with liver damage or cirrhosis.
Baclofen must be titrated up and down when starting and stopping to minimize the risk of side effects. Side effects at all are infrequent, but the most common ones are fatigue, insomnia, dizziness, and nausea. They usually only happen on dose increases, and pass within a day or two. Recurrent side effects can be mitigated by slowing down your titration. Baclofen has no known permanent or long-term side effects.
Effortless Indifference — Dr. Ameisen’s Journey
In 2008, Weill-Cornell Hospital cardiologist and former first physician to the French Prime Minister, Dr. Olivier Ameisen, discovered a miraculous solution to his chronic over-drinking after 8 stints in rehab and a total of over 5000 AA meetings.
Dr. Ameisen began experimenting on himself with baclofen, a decades-old drug known to be safe at high doses that had shown recent promise in everything from panic attacks to cocaine addiction to alcoholism. After two years, Ameisen had reached his effective dose, achieving total, effortless indifference to alcohol.
“I was not just abstinent with regard to alcohol: I was effortlessly indifferent to it. Everyone noticed the change in me. They remarked on how cleareyed and vital I looked. Friends and acquaintances said: ‘You are like a new man.’Sixteen months after my last drink, I put my new regimen to the challenge - and have discovered that I can have a glass or two of champagne, or a vodka tonic, but not crave any more. Five years on, and baclofen has both freed me of all craving for alcohol and resolved the underlying disorder - overwhelming anxiety - that made me vulnerable to addiction. By completely suppressing my addiction, baclofen saved my life.”
“If it was willpower alone anyone would do it. The medication that they provided added the additional chemical change that I needed to take control. It’s changed my life.”
— Damian
Ready to Kick Your Drinking Habit?
Our LifeBac providers are available to get your prescription approved right away–just click the link below to fill out our intake form, and we’ll reach out shortly to start the process.